A new report says climate change is taking a toll on public health and related costs. The study looked at 10 climate-sensitive events in 2012, such as Hurricane Sandy in New York and New Jersey, and came up with a dollar amount in the billions. The report comes ahead of a planned global climate strike Friday.
The Natural Resources Defense Council and the University of California, San Francisco, released a study Wednesday on the health costs of climate change. Study lead author Dr. Vijay Limaye, a scientist in NRDC’s Science Center, says the report connects health impacts in the 10 case studies — deaths and illnesses — to health costs.
“So we estimated about $10 billion in health damages inflicted by just these 10 climate-sensitive case study events. That’s from about 900 deaths; 21,000 hospitalizations; and 18,000 emergency room visits. So these are the types of costs that folks are paying for right now. And this work signals tens to hundreds of billions of dollars in additional health-related costs in the future if we fail to act,” Limaye says. “We estimated that about two-thirds of the illness costs were shouldered by Medicare and Medicaid patients, which aligns with our understanding that younger and older folks are particularly vulnerable to the health harms posed by climate change.”
“And I think in an era of concern about rising health care costs, this is a really important message. Climate change is adding to the health-care cost burden,” says Max. “And we need to be doing things to both reduce the impact of climate change but also to make the system more nimble in terms of responding, the emergency room… emergency care services, and so forth. So I think that that’s a message that we’re hoping will resonate with policymakers.”
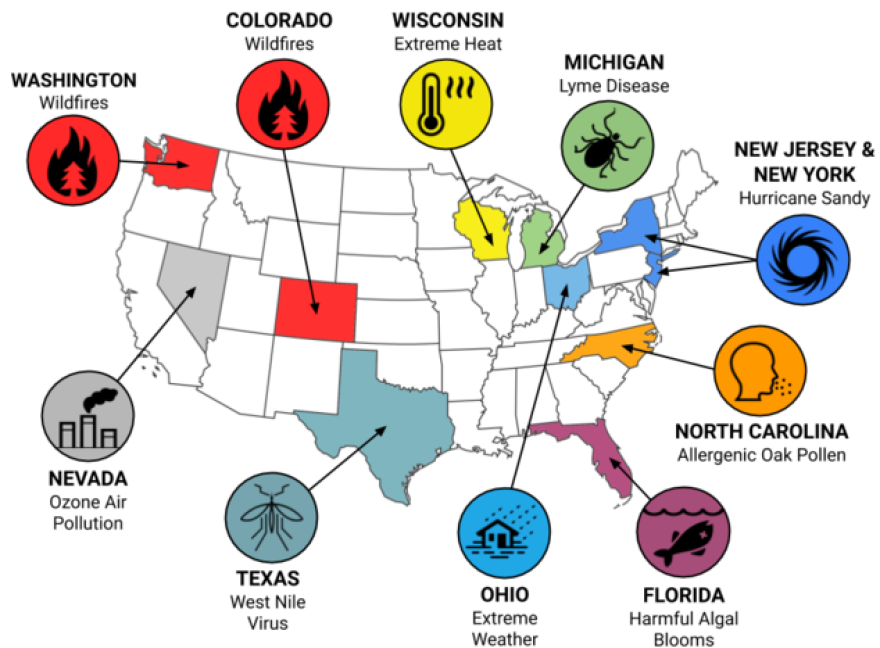
Dr. Wendy Max is the study’s co-author and a professor at the University of California, San Francisco Institute for Health & Aging. The 10 case studies include wildfires in Colorado and Washington; ozone air pollution in Nevada; extreme heat in Wisconsin; harmful algal blooms on the Florida coast and Hurricane Sandy in New Jersey and New York.
“The most costly event was Hurricane Sandy, which resulted in 273 deaths and $3.1 billion in health care costs, followed by wildfires in Washington state, which cause 245 deaths and $2.3 billion in health care costs,” Max says. “And this is just the tip of iceberg. We know this is an underestimate of the health cost.”
Again, Limaye.
“For an event like Hurricane Sandy, the public health science is still catching up to what actually happened on the ground as a result of that storm almost seven years ago,” Limaye says. “So we incorporated a recent study published in 2019 on pregnancy complications caused by the storm.”
The study also examined mosquito-borne West Nile Virus in Texas and outbreaks of tick-borne Lyme disease in Michigan.
“Michigan is a low incidence state for Lyme disease, but it’s a state in which the incidents of that vector-borne disease transmitted by ticks has expanded over the last decade or so,” says Limaye. “There are other states that have higher incidents of Lyme, but we wanted to capture a range in terms of the intensity of the exposure and health outcomes.”
Limaye says the NRDC’s research shows that health-related costs added at least another 26 percent to the national price tag for 2012 severe weather-related damages. And he says the study weaves together more than three dozen data sources.
“National assessments of disasters and extreme events impacts have been focused on counting the things are insured or repaired, like homes, office buildings, roads or crops,” says Limaye.
He says there is no publicly-available unified tracking of climate-sensitive health outcomes.
“Studies like this show that we’ve got to expand the conversation on climate change to include the profound suffering and expensive health costs that we can avoid by cutting climate pollution and investing in community preparedness,” Limaye says.
Dr. Jeremy Hess is an Associate Professor and Director of the Center for Health and the Global Environment at the University of Washington. He also is an emergency room physician, and was not involved in the study.
“Impacts from many of these exposures can be blunted, often substantially, through aggressive public health action,” Hess says. “That said, we’re not investing in public health preparedness to the extent that we need to to anticipate and prepare for and reduce the impact of these exposures.”
Dr. Jay Lemery is a professor at the University of Colorado School of Medicine. Also an emergency room physician, he says the report brings to light another need.
“We need to train medical professionals in fluency and a common vocabulary on these issues.,” says Lemery. “How do we do that? We really need to tackle it from– and many people on the expert panel are involved with this — is tackle it from all aspects of medical education through codifying a curriculum that we can implement in the schools of medicine and schools of public health as well as train physicians through intense dedicated fellowships as well as continuing medical education opportunities through the different medical colleges across all sectors, not just in emergency medicine, but really all care providers, because there’s still a conspicuous absence in the clinical community on these issues.”
The study is published in the journal GeoHealth.